Abstract
Background: Vitamin D is synthesized by exposure to sunlight or provided as a diet and metabolized in the liver to 25-hydroxyvitamin D, the main circulating form of vitamin D. It is known to play an important role in calcium and bone homeostasis. Moreover, it is also associated with antitumor effects through modulation of inflammation, cell proliferation, cell differentiation, angiogenesis, and apoptosis. Indeed, several recent studies have shown that vitamin D deficiency is associated with poor prognosis in many types of cancer, including hematological malignancies. However, the prognostic value of vitamin D in peripheral T-cell lymphoma (PTCL) remains unclear. In this study, we aimed to evaluate the prognostic value of vitamin D levels in newly diagnosed patients with PTCL.
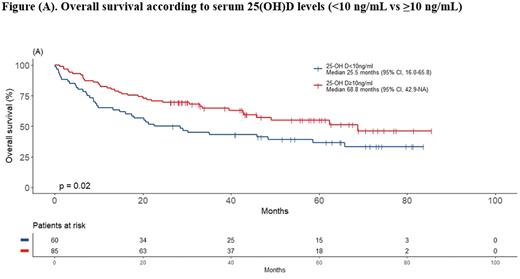
Methods: Between March 2015 and May 2020, 191 patients were newly diagnosed with PTCL at Asan Medical Center, Seoul, South Korea. After excluding patients with no baseline vitamin D level and cutaneous T-cell lymphoma and NK/T-cell lymphoma, 145 patients were included in this analysis. Overall survival (OS) was defined as the time from the date of diagnosis to any cause of death. Univariate analysis included key baseline characteristics and candidate prognostic factors, including age, sex, Eastern Cooperative Oncology Group Performance status (ECOG PS), International Prognostic Index (IPI) score, vitamin D, and CRP. Vitamin D deficiency was defined as 25-(OH)D < 10 ng/mL. In the multivariate analysis, variables that showed potential association with OS (p-value < 0.2) in the univariate analyses were included.
Results: The median age at diagnosis was 60 years (range, 16-85), 89 patients were male (61.4%), 135 patients had ECOG PS of < 2 (93.1%), and 117 patients had advanced stage disease (80.7%). PTCL, not otherwise specified (PTCL-NOS) was the most common pathologic subtype (n=74, 51.0%) followed by angioimmunoblastic T-cell lymphoma (AITL) (n=38, 26.2%), and anaplastic large cell lymphoma (ALCL) (n=33, 22.8%). Median 25-(OH)D serum level was 11.7 ng/mL (range, 1.7-48.8ng/mL) and 60 patients had vitamin D deficiency (41%). Higher proportion of patients with vitamin D deficiency had elevated LDH (68.3% vs. 47.1%, P = 0.02) and elevated CRP (77.6% vs. 58.3%, P = 0.03). With a median follow-up duration of 30.3 months (95% CI, 1.6-77.4 months), the median OS was 48.5 months in entire patients. Patients in the vitamin D deficiency group were significantly associated with worse OS compared with the non-vitamin D deficiency group, with a median OS of 25.5 months vs. 68.8 months (P = 0.02), respectively. In the univariate analysis, IPI score and vitamin D showed potential association with OS (P < 0.20). In the multivariate analysis, vitamin D was independently associated with OS with a hazard ratio of 1.63 (95% CI, 1.03-2.58, P = 0.04).
Conclusion: In this study, we demonstrated that vitamin D deficiency is significantly associated with poor survival outcomes in patients with peripheral T-cell lymphoma. The prognostic significance of vitamin D in PTCL patients deserves further validation in future studies.
Disclosures
Yoon:Samyang: Honoraria, Research Funding; Novartis: Honoraria; Boryung: Honoraria, Research Funding; Pharos iBio: Consultancy; Sanofi: Research Funding; Celltrion: Honoraria, Research Funding; Beigene: Research Funding; Amgen: Honoraria; BMS: Honoraria; Takeda: Honoraria; Roche: Honoraria; GI Cell: Consultancy; Ab Clone: Consultancy; Janssen: Honoraria, Research Funding; Kirin: Honoraria, Research Funding; GSK: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal